












Kliniskt Manligt Bäcken (KMB) Mk 2 - Avancerad
Skin Tone
Model
Vår anatomiskt noggranna modell är en idealisk plattform för undervisning och lärande av manlig bäckenundersökning och diagnos. Den användarvänliga designen kombinerad med tydliga anatomiska landmärken och en rad patologier skapar en realistisk träningserfarenhet för studenter på alla nivåer inom vårdutbildning. Utvecklat i samarbete med: The Clinical Skills Resource Centre, University of Liverpool, UK Imperial College, London, UK Guys Hospital, London, UK Southmead Hospital, Bristol, UK University of Southampton, UK
Overview
- Anatomically accurate male simulator that allows for realistic practice of the male pelvic exam
- 7 supplied modules give a wide variety of pathologies to identify
- A Foreskin Pack is included to practice procedures on both circumcised and uncircumcised anatomy
Realism
- Mjukdelskönsorgan och bukvägg
Versatility
- Mjukdelsinlägg kan tas bort och bytas ut
- Kan användas i två positioner: stående och liggandes på rygg
Cleaning
- Hudytan kan tvättas med tvål och vatten
Safety
- Latexfri
Simulated Patient
- The Clinical Male Pelvic Trainers can be used with a simulated patient
Anatomy
- Buk, bäcken och könsorgan
Ljumskens anatomi med tydliga anatomiska landmärken:
- Spina iliaca anterior superior
- Blygdbensfog och tuberculum pubicum
Könsorganet består av:
- Penis - både omskuren och icke-omskuren
- Pung - som innehåller testiklar med bitestikel och sädesledare
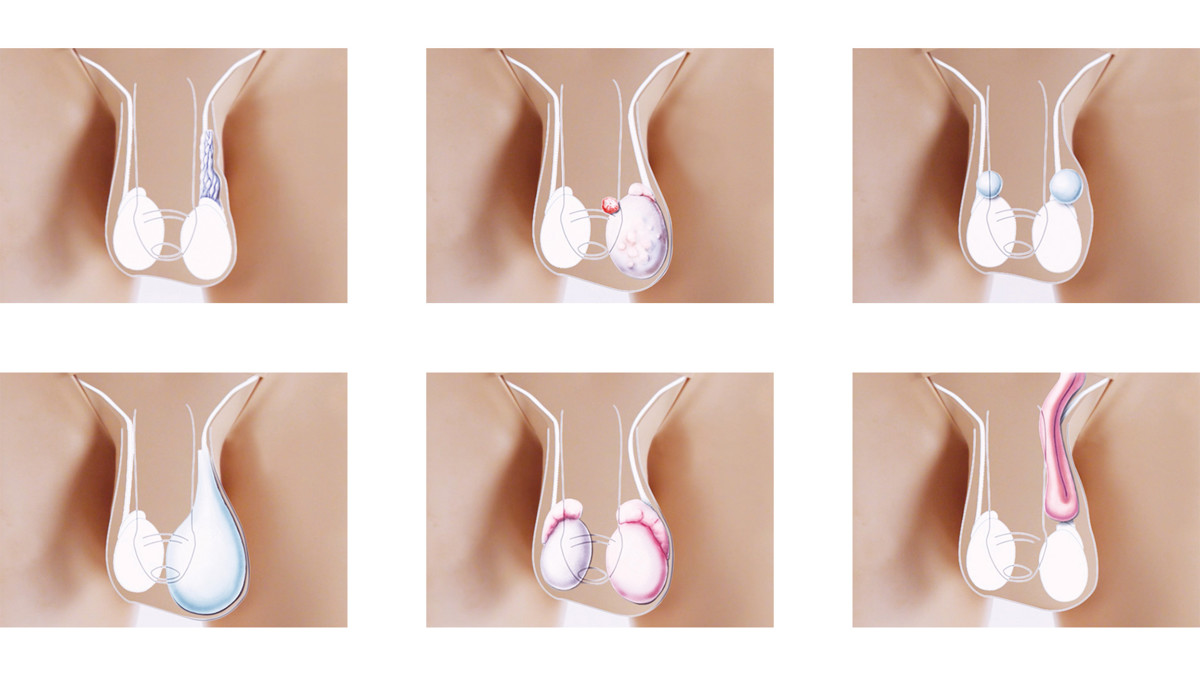
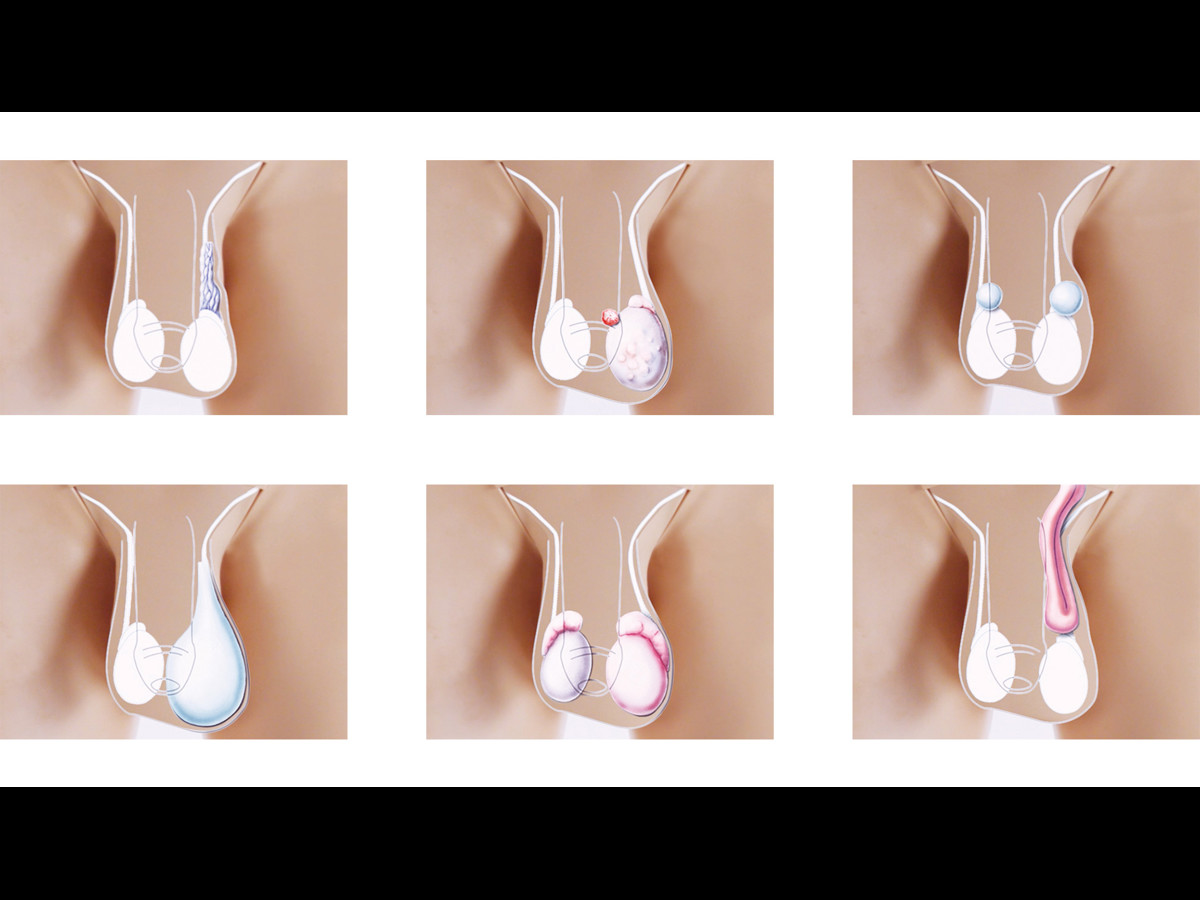
Patologier:
- Testikeltumör och peniscancer
- Spermatocele
- Varikocele
- Orkit/bitestikel-orkit
- Hydrocele
- Ljumskbråck
Skills Gained
- Korrekt undersökningsförfarande för manliga bäcken
Undersökning och utvärdering av:
- Normal anatomi
- Testikulära abnormiteter
- Buk- och bäckensmärta
- Torr kateterisering
Jämförelse |
Produktnr. |
|
|---|---|---|
| Färdigheter | 60951 | 60950 |
| Korrekt undersökningsförfarande för manliga bäcken | Yes | Yes |
| Undersökning och utvärdering av: | ||
| Normal anatomi | Yes | Yes |
| Testikulära abnormiteter | Yes | Yes |
| Buk- och bäckensmärta | Yes | Yes |
| Torr kateterisering | Yes | No |
Product Contains

Augmented Reality Mat for CMPT
-
Light
-
Dark

KMB Mk 2 Modul 1: Normal
-
Light
-
Dark

KMB Mk 2 Modul 2: Varikocele
-
Light
-
Dark

KMB Mk 2 Modul 3: Tumörer
-
Light
-
Dark

KMB Mk 2 Modul 5: Hydrocele
-
Light
-
Dark

KMB Mk 2 Modul 6: Orkit/bitestikel-orkit
-
Light
-
Dark

KMB Mk 2 Modul 7: Ljumskbråck
-
Light
-
Dark

KMB Mk 2 Bukinsats
-
Light
-
Dark

KMB Mk 2 Förhud (x2)
-
Light
-
Dark

KMB Mk 2 Modul 4: Spermatocele
Jämförelse |
Produktnr. |
||
|---|---|---|---|
| Vad ingår | 60951 | 60950 | |
| 60952 | KMB Mk 2 Modul 1: Normal | Yes | Yes |
| 60953 | KMB Mk 2 Modul 2: Varikocele | Yes | No |
| 60954 | KMB Mk 2 Modul 3: Tumörer | Yes | No |
| 60955 | KMB Mk 2 Modul 4: Spermatocele | Yes | No |
| 60956 | KMB Mk 2 Modul 5: Hydrocele | Yes | No |
| 60957 | KMB Mk 2 Modul 6: Orkit/bitestikel-orkit | Yes | No |
| 60958 | KMB Mk 2 Modul 7: Ljumskbråck | Yes | No |
| 60959 | KMB Mk 2 Bukinsats | Yes | Yes |
| 60960 | KMB Mk 2 Blygdben | Yes | Yes |
| 60961 | KMB Mk 2 Förhud (x2) | Yes | Yes |
| - | Nedre torso | Yes | Yes |
| - | Stödbas | Yes | Yes |
| - | Väska (modell) | Yes | Yes |
| - | Väska (moduler) | Yes | No |
| - | LED-penna | Yes | No |
Works with the following products:
-
Light
-
Dark

KMB Mk 2 Modul 1: Normal
-
Light
-
Dark

KMB Mk 2 Modul 2: Varikocele
-
Light
-
Dark

KMB Mk 2 Modul 3: Tumörer
-
Light
-
Dark

KMB Mk 2 Modul 4: Spermatocele
-
Light
-
Dark

KMB Mk 2 Modul 5: Hydrocele
-
Light
-
Dark

KMB Mk 2 Modul 6: Orkit/bitestikel-orkit
-
Light
-
Dark

KMB Mk 2 Modul 7: Ljumskbråck
-
Light
-
Dark

KMB Mk 2 Bukinsats
-
Light
-
Dark

KMB Mk 2 Förhud (x2)
References
National Organisation of Nurse Practitioner Faculties, Nurse Practitioner Core Competencies Content, 2017 Independent Practice Competencies p.14 3.b Uses advanced health assessment skills to differentiate between normal, variations of normal and abnormal findings. 3.c Employs screening and diagnostic strategies in the development of diagnoses.
AAFP Recommended Curriculum Guidelines for Family Medicine Residents, Men’s Health Reprint No. 257, 2016 p.3 Perform a comprehensive male physical examination, including urogenital... p.5 the resident should demonstrate the ability to independently perform or appropriately refer the following: 1. Male-specific examination a. Penile/testicular/scrotal exam c. Hernia/inguinal exam
AAMC (2008) - Recommendations for Pre-clerkship Clinical Skills Education for Undergraduate Medical Education p.26Appendix 5: Patient Examination. Perform testicular exam and describe examination process and findings
CPMEC Australian Curriculm Framework for Junior Doctors v 3.1, 2012, p.7: History and Examination: Performs a comprehensive examination of all systems; Elicits symptoms & signs relevant to the presenting problem or condition. Discriminates between the possible differential diagnoses relevant to a patient's presenting problems or conditions
RACGP Curriculum for Australian General Practice 2016, SH16 Sexual and Reproductive Health Essential skills for general practitioners to develop and maintain include: ...undertaking a sensitive genital examination, if appropriate, to assess risk, determine appropriate assessment, investigation and management
Medical Deans' Clinical Assessment Blueprints for the medical graduate 4. Conducts ... organ(s)/system specific physical examination as appropriate. 5. Integrates the information obtained to arrive at an appropriate diagnosis and differential diagnosis.
Competence and Curriculum Framework for the Physician Assistant 2012, p 12 2.3.5 ...Perform a physical examination tailored to the needs of the patient and the demands of the clinical situation, including ...male uro-genital examination
Specialty Training Curriculum for Core Medical Training, 2013 p.86: Perform full examination including...scrotum, male urethra
The UK Foundation Programme Curriculum 2016. p.9: obtains history, performs clinical examination, formulates differential diagnosis and management plan (FPC 11)
The Intercollegiate Surgical Curriculum, Urology Surgery, Aug 2015 p.20 Recognise the common malignant and potentially malignant conditions of the penis...Diagnose and manage patients presenting with scrotal symptoms such as hydrocele, epididymal cyst, varicocele
Outcomes for Graduates 2018, General Medical Council, p.16 Diagnosis and medical management: 14b. safely and sensitively undertake an appropriate physical examination ...interpret findings from physical examinations...synthesise findings from the history, physical and mental state examinations and investigations ... and make proposals about underlying causes or pathology
RCN Competencies - Advanced Nurse Practitioners, 2012, p.4 ...receiving patients with undifferentiated and undiagnosed problems and making an assessment of their health care needs, based on highly-developed nursing knowledge and skills ... such as physical examination
Guidance for Satisfactory Progression at ARCP panels for GP Specialty Trainees, 2016 p.6 ... evidence of competence of intimate examinations which includes ...the full range of ... male genital examinations.
Can trainees practice catheterization on the Clinical Male Pelvic Trainer?
Yes, the CMPT can be used to practice dry catheterization techniques. However, if you’re looking to do more extensive training in this procedure, the Male Catheterization Trainer range may be more suited to your training needs.
Is it possible to use transillumination on the male pelvic simulator to identify pathologies?
Using the supplied LED Pen Torch, transillumination can be performed on the scrotum. For example, on Module 4, illuminating the scrotum will allow trainees to visually identify the two Epididymal Cysts.
Can the CMPT be used to simulate cancer in male genitalia?
Yes, Module 3 can be used in the identification of two presentations of cancer. The left testicle has a solid mass with an irregular surface, representing a Testicular Tumour or Teratoma. The penis has visual lesion, the lump is solid and has an irregular surface, representing Penile Cancer.












